Trending Now

Get moving and get rewarded!
Seniors get to start exercising and at the end of the session, they are given a complimentary...
National Heritage Board launches first Heritage Activation Node in Katong-Joo Chiat
Working with community partners, there are over 25 programmes for everyone to enjoy. The...
Senior, residents in Chong Pang embrace digital literacy
They explored online shopping experiences through hands-on activities at the event, which was part...
More middle-aged and older men seeking male breast reduction in Singapore
According to a doctor, the mean age was 33, however in recent years, older male patients above 42...
Latest Articles
Health

Get moving and get rewarded!
Seniors get to start exercising and at the end of the session, they are given a complimentary meal. Get moving and get rewarded. St Luke’s Eldercare (SLEC) has introduced a programme called WE! (Workout Empowerment!), an incentive-based fitness programme to get...

More middle-aged and older men seeking male breast reduction in Singapore
According to a doctor, the mean age was 33, however in recent years, older male patients above 42 have increased, with the oldest being 70. Dr Ivan Puah, a Singapore Ministry of Health-accredited liposuction doctor with years of experience in gynecomastia and...
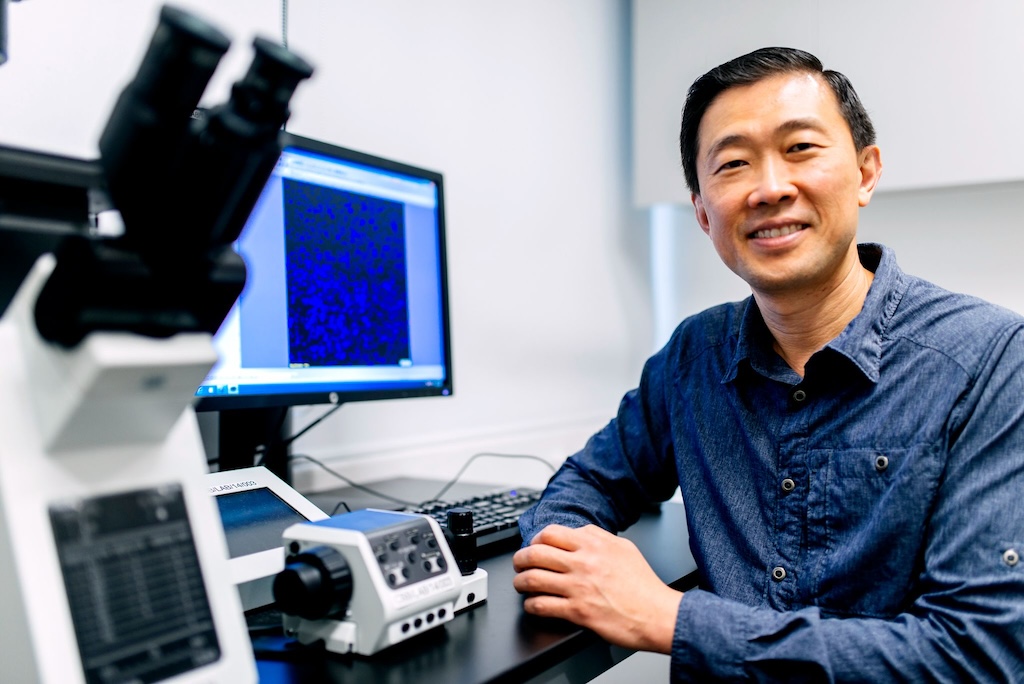
First clinical cancer drug screening test
It looks to personalise treatments by improving the efficiency of chemotherapy regimes through testing using patients’ own cancer cells. Biotechnology and medical innovation company, Invitrocue, has achieved a breakthrough in clinical drug testing with...
View All
Inspiring Figures

Getting a degree
The oldest graduand in this year’s Singapore University of Social Studies convocation event was 73-year-old Tan Tiang Wang. This year’s Singapore University of Social Studies (SUSS) convocation event had the largest graduating cohort with nearly 3,000...

Parkour for seniors
Two seniors share their experiences and that age shouldn’t be a limit. It is a little after 9am on a weekday and the outdoor fitness station area surrounded by several HDB flats in Ang Mo Kio has been turned into a parkour training ground. Ten women are rolling...
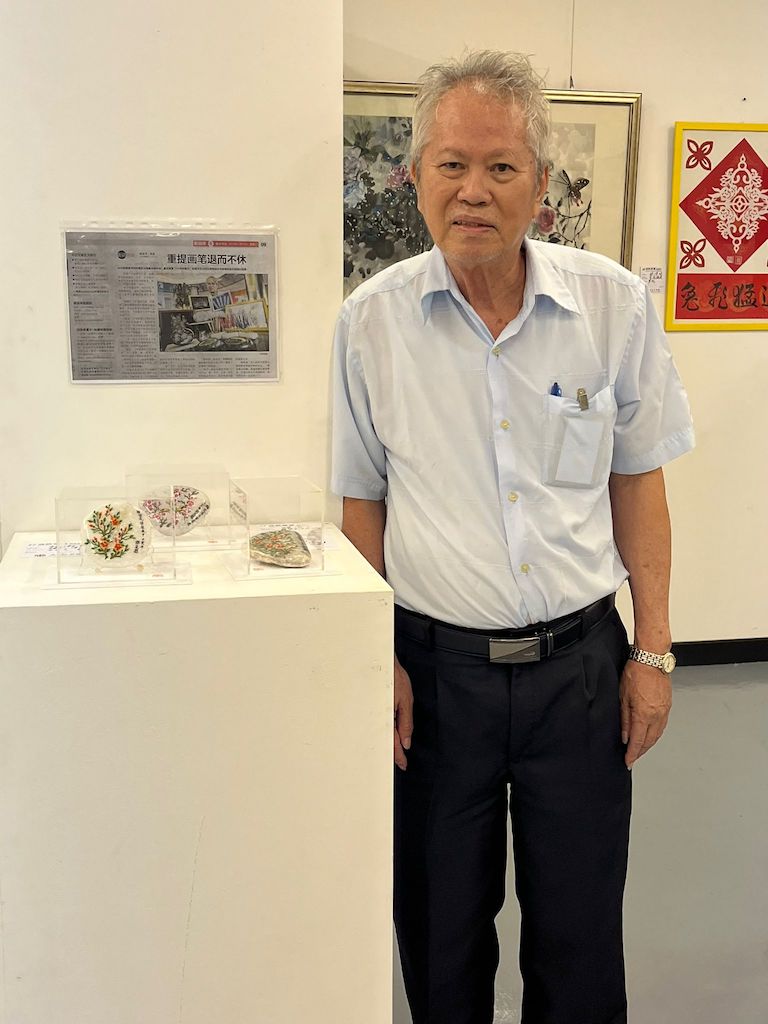
Pebble art
They may be common objects but to Lim Teo Cher, they mean a whole lot more. We see them in our gardens and in our potted plants, as well as along walkways. We don’t think much about these pebbles. For 73-year-old Lim Teo Cher, he looks at these sometimes oddly...
View All
Finance

Online nomination of beneficiary
Previously Prudential policyholders had to submit a hard copy via post or in person at the customer service centre. Want to nominate your beneficiary for your Prudential Singapore policy? Now you can online. Prudential is the first insurer here in Singapore to...

First accident plan to cover multi-stage dementia
AIA Centurion PA Plan provides comprehensive coverage including value added services such as home care, health screening and teleconsultations. AIA Singapore will be a launching a personal accident insurance plan that covers neurological diseases like...

Three in five people have a side job to help make ends meet
Respondents to the survey cited dealing with the rising cost of living and inflation as the top motivation for starting a side job. Almost three in five (59 percent) people have a side job, and the top reason for doing so is to make ends meet (61 percent). This...
View All
Latest Articles
Health
View All

Get moving and get rewarded!
Seniors get to start exercising and at the end of the session, they are given a complimentary meal. Get moving and get rewarded. St Luke’s Eldercare (SLEC) has introduced a programme called WE! (Workout Empowerment!), an incentive-based fitness programme to get...

More middle-aged and older men seeking male breast reduction in Singapore
According to a doctor, the mean age was 33, however in recent years, older male patients above 42 have increased, with the oldest being 70. Dr Ivan Puah, a Singapore Ministry of Health-accredited liposuction doctor with years of experience in gynecomastia and...
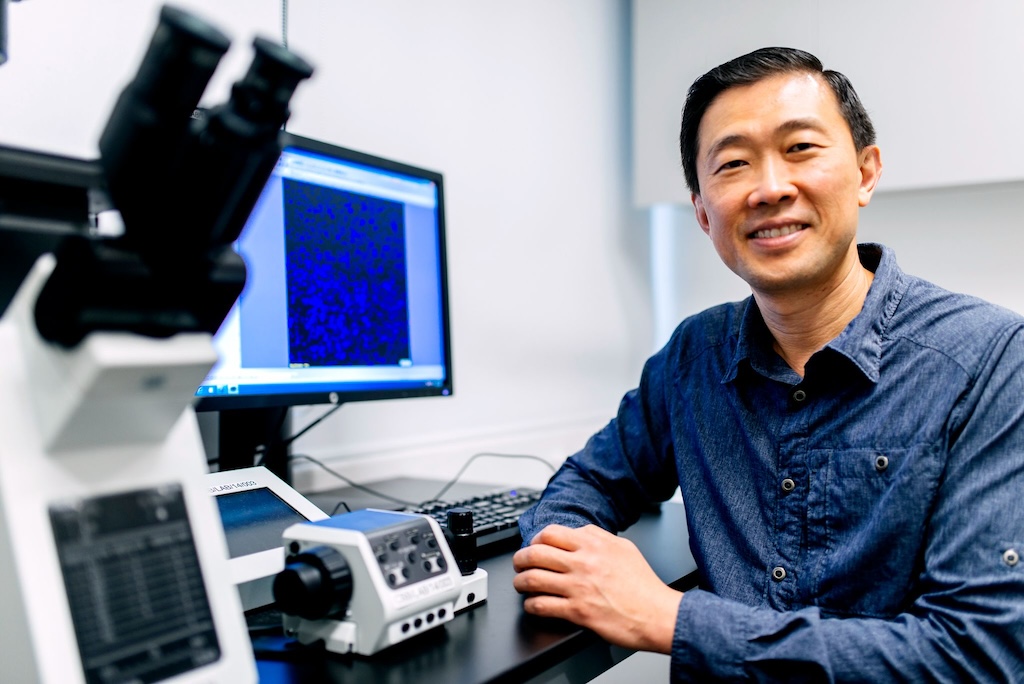
First clinical cancer drug screening test
It looks to personalise treatments by improving the efficiency of chemotherapy regimes through testing using patients’ own cancer cells. Biotechnology and medical innovation company, Invitrocue, has achieved a breakthrough in clinical drug testing with...
Inspiring Figures
View All

Getting a degree
The oldest graduand in this year’s Singapore University of Social Studies convocation event was 73-year-old Tan Tiang Wang. This year’s Singapore University of Social Studies (SUSS) convocation event had the largest graduating cohort with nearly 3,000...

Parkour for seniors
Two seniors share their experiences and that age shouldn’t be a limit. It is a little after 9am on a weekday and the outdoor fitness station area surrounded by several HDB flats in Ang Mo Kio has been turned into a parkour training ground. Ten women are rolling...
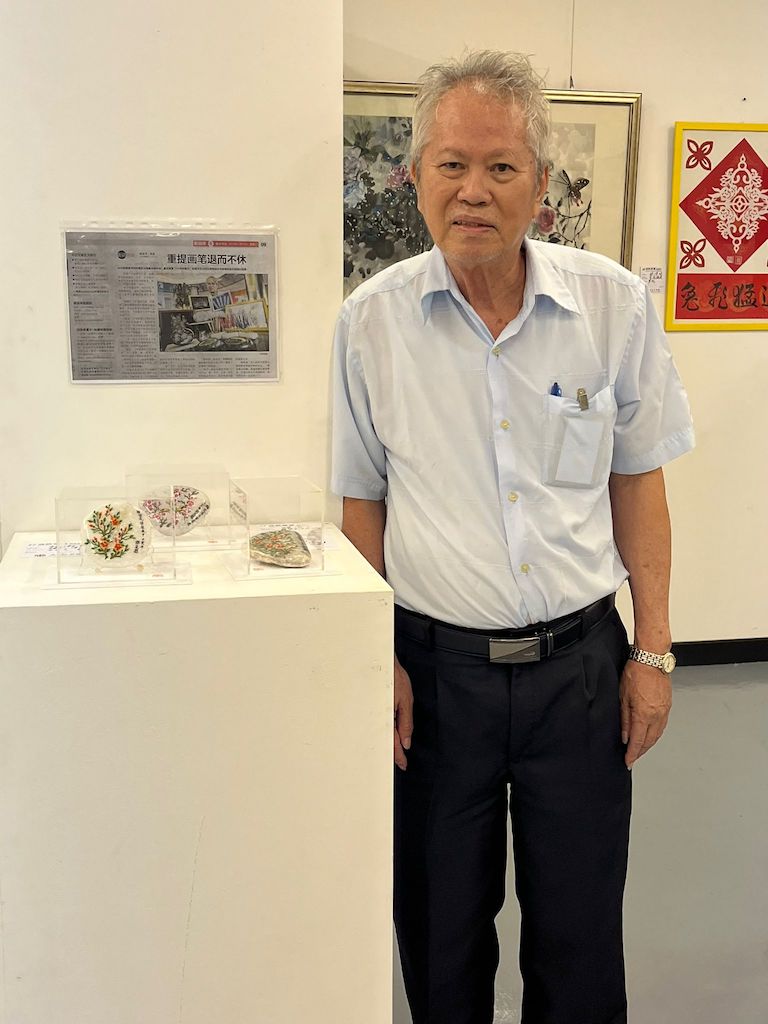
Pebble art
They may be common objects but to Lim Teo Cher, they mean a whole lot more. We see them in our gardens and in our potted plants, as well as along walkways. We don’t think much about these pebbles. For 73-year-old Lim Teo Cher, he looks at these sometimes oddly...
Finance
View All

Online nomination of beneficiary
Previously Prudential policyholders had to submit a hard copy via post or in person at the customer service centre. Want to nominate your beneficiary for your Prudential Singapore policy? Now you can online. Prudential is the first insurer here in Singapore to...

First accident plan to cover multi-stage dementia
AIA Centurion PA Plan provides comprehensive coverage including value added services such as home care, health screening and teleconsultations. AIA Singapore will be a launching a personal accident insurance plan that covers neurological diseases like...

Three in five people have a side job to help make ends meet
Respondents to the survey cited dealing with the rising cost of living and inflation as the top motivation for starting a side job. Almost three in five (59 percent) people have a side job, and the top reason for doing so is to make ends meet (61 percent). This...


